Shoulder pain is a very common and debilitating issue that affects people of all ages and backgrounds and most of the time in multiple stages throughout life.
The shoulder is one of the most mobile and complex joints in the human body, making it susceptible to various types of pain and dysfunction due to its complex anatomy and ability to move multidirectional.
In this deep dive into shoulder pain, we will explore the anatomy of the shoulder, the common causes and reasons of shoulder pain, potential treatment options, and preventive measures to give us a well rounded understanding of the complex shoulder joint.
Anatomy of the Shoulder
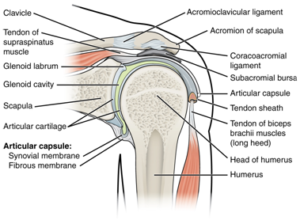
The shoulder joint (also known as the glenohumeral joint) is a ball and socket type joint, similar to that of the hip, that consists of three primary bones: the humerus (upper arm bone), the scapula (shoulder blade), and the clavicle (collarbone).
The head of the humerus fits into the shallow socket of the scapula, forming the glenohumeral joint. This is then held into the socket via active and passive structures. The active structures being the Rotator Cuff and the passive structures are the ligaments and joint capsule of the shoulder.
These key structures are involved in the shoulder’s mobility and overall function, and it is damage, overuse or underuse of one of these structures that can cause acute or chronic shoulder pain and dysfunction.
First let’s take a look at the active stabilizers of the shoulder; The Rotator Cuff. The rotator cuff is a group of four muscles that act as a suction cup around the head of the humerus. These muscles are constantly working together as one unit throughout normal shoulder movement to stabilize the humeral head in the socket and produce smooth movement. These muscles include the supraspinatus, infraspinatus, teres minor, and subscapularis.
When movement is produced friction occurs between the tendons and bones. In order to reduce this friction we have structures called Bursa which are filled with fluid and lubricate and reduce overall friction between the moving tendons of the shoulder.
Now let’s take a look at the passive stabilizers of the shoulder, starting with the Glenoid Labrum. The labrum is a rim of cartilage that wraps around the circumference of the glenoid fossa (the socket) in order to deepen the socket and provide a little more support for the moving humeral head.
This is then supported with the joint capsule, the joint capsule is an envelope surrounding the joint filled with synovial fluid which is required for smooth movement.
The bones which make up the shoulder joint are connected via ligaments. Which is a dense connective tissue that connects bone to bone – providing stability and support between the main bones of the shoulder.
Now we’ve taken a look at the anatomy of the shoulder, we can understand that there are many different structures around the shoulder which can become dysfunctional and as a result throughout the normal movement of the shoulder and cause pain.
Rotator Cuff Injuries:
Rotator cuff injuries come in a variety of forms, from acute traumatic injuries such as tears or strain ,of the rotator cuff muscles, or can be more of a chronic condition from overuse and degeneration and resulting in ongoing pain and limited mobility.
Frozen Shoulder (Adhesive Capsulitis): A condition characterized by stiffness and restricted range of motion due to inflammation and thickening of the shoulder capsule. This can be debilitating and happen post surgery, after a traumatic incident or be idiopathic (of unknown origin).
Bursitis: Inflammation of the bursa can occur due to repetitive overhead motions or direct trauma, causing pain and swelling in different areas of the shoulder joint. Typically this is accompanied by night pain, a burning sensation and weakness in the movements of the shoulder.
Tendon Related Pain: Tendon related pain is usually due to an overuse or an overloading of the muscles of the shoulder which can cause inflammation around the tendon and microdamage to the tendon itself.
Arthritis is a painful condition that occurs over time with natural degenerative changes to the joint. Arthritis is a normal process of aging however can be painful and debilitating if not treated appropriately.
Neck related shoulder pain: In some cases, shoulder pain can often be referred from the joints, muscles or nerve roots that stem from the cervical spine (neck). This can lead people to believe that shoulder pain is coming from the structures in the shoulder, however it can often be referring from a different location, making it difficult to treat and diagnose without an experienced Physiotherapist.
Shoulder Instability: Shoulder instability occurs due to the disengagement, inactivity or overactivity of the muscles of the shoulder, due to a shallow ball and socket joint as spoken about previously, due to a traumatic injury which has caused structural damage and can be a debilitating and frustrating injury which requires an accurate diagnosis and management plan to rehabilitate.
This is only scratching the surface when it comes to the shoulder joint, there is still so much we are learning through research and there is still so much unknown. The shoulder is a very complex joint which does not have a one size fits all solution. At Team Elite Health we have the skills necessary to accurately diagnose, manage and rehabilitate shoulder related pain and injuries to ensure that quality of life is restored and you are able to return back to full function of daily life, whatever that may be for you.